Running News Daily
Running News Daily is edited by Bob Anderson. Send your news items to bob@mybestruns.com Advertising opportunities available. Train the Kenyan Way at KATA Kenya and Portugal owned and operated by Bob Anderson. Be sure to catch our movie A Long Run the movie KATA Running Camps and KATA Potato Farms - 31 now open in Kenya! https://kata.ke/
Index to Daily Posts · Sign Up For Updates · Run The World Feed
Running May Have Saved My Life
Nearly 50 years ago I fell in love with running. I was far from a natural. When I was 8 years old, I was struck by an illness that left me with pneumonia in both lungs with one lung being collapsed. I survived that but was left with asthma that persists to this day. This was unfortunate as I loved sports. Asthma more or less disqualified me from participating in “running sports, " leaving me only with baseball as something I could do relatively comfortably.
In high school, I wanted to try wrestling. I figured that I could handle three 2-minute periods. However, I would soon learn that a lot of the training involved running and I struggled mightily to keep up with the other kids early in the season. The next season I hit upon the idea to ask our cross-country coach if I could train with that team, though not be part of the team. In this way, I could be conditioned before the start of wrestling season. And during wrestling season, I would show up two hours before the match to check my weight and run 2-4 miles before weigh-in.
I graduated high school, but the running never stopped. I ran every weekend (4-10 miles each day) for decades. Running was so important to me that when setting up one of my company offices in Japan, I purposely chose a location in a place with a suitable place to run, near the Emperor’s Palace near Tokyo Station. The palace is surrounded by a circular (3km) moat that is a popular running destination. My ritual was that after a week of business, I would do four laps around the palace and then fly home to San Francisco.
Though I loved running I was never interested in racing until about age 50. In 2010, my new son-in-law invited me to join him in a 5K fun run in Lafayette. Passing all those 20-year-olds was all I needed to get the “bug.” I went on to run many dozens of races over the next years, mostly marathons, an ultra, and a triathlon. I was in the best shape of my life, rarely got sick, and was at the top of the world. That would change dramatically.

In 2013, I started noticing that on some days I would experience a strange fatigue that required me to take a walking break. I remember one day that I cut one of my runs short because I was disgusted with my performance. I kept my running clothes on and decided that I would try again later that day. That was the time I set a new PR for that training course. Something was not right, and these episodes of fatigue were increasing in frequency.
The last marathon I ran was in April 2016, a miserable affair clocking in a 4:53. By September, I couldn’t run a mile without a break. I complained to every doctor I met that “something was wrong”, but the standard response was that I was just getting older and I needed to lower my expectations. Even a cardiologist I had seen 10 years earlier told me that there was nothing wrong with me and even quipped “Guys like you are bad for business.” I wasn’t amused.
Finally, in 2019, my asthma doctor recommended a private practice cardiologist in Los Altos who might be willing to work with me. She spent two hours examining me, including an EKG and blood work. She found no problems but listened to my story about my newfound exercise intolerance. She said the only way to get to the bottom of it was to put me under a cardiac stress test.
I showed up at the hospital and they were ready for me. My doctor was there along with two technicians: one to operate the treadmill and monitor the EKG, and one with an echocardiogram scanner for a pre- and post-test scan of my heart. About 15 minutes into the test, about the same interval that I would experience fatigue during a run, the EKG technician exclaimed “Doctor!” and ran out of the room. The doctor told me to stop, asked me if I was OK, and asked me to lie down and have the other technician scan me.
The EKG technician quickly reappeared with defibrillating paddles and was stunned that I was calmly talking to the doctor. The cause of my fatigue was now clear– I was having a heart attack. A very deadly one at that, called Ventricular Tachycardia (VT) in which the top and bottom chambers beat at different rates causing your heart to stop pumping.
Now that the mystery was solved (I was not “fine”), we needed to identify the cause of this electrical misfiring. I was then directed to a cardiac electrophysiologist (EP) that specializes in this sort of disorder. He also took several hours to explain that there are nearly a dozen potential causes of this, and nearly all of them treatable. There was one (the least likely) however, that was not so easily treatable.
As it turns out, the least likely one Cardiac Sarcoidosis, was the one. This is a rare auto-immune disease that typically attacks the lungs but in even rarer cases can attack the heart. Lucky me. These “attacks” leave scar tissue on the heart that disrupts the normal electrical activity of the heart. My EP regretted telling me that this was out of his skill area and needed to refer me to Stanford where they have a cardiologist that specializes in this.
My experience at Stanford was great where a team of cardiologists took care of me. The first step was to see if the VT response to exercise was repeatable (it was). The second step was to confirm that sarcoidosis auto-immune cells were present in my body. The result of that test was positive. The cells were present, but the good news was that they were no longer in my heart and were “dormant.” But the damage was done. The final step was to install an implantable cardiac defibrillator (ICD) in my chest that has two wires screwed into the side of my heart. In case of a sustained VT episode, the ICD would automatically shock me back into rhythm.
My ICD was installed on February 12, 2020 shortly before the Covid lockdown. I cleared to begin running after about six weeks which I gleefully did after eight months of no running and four years of poor running. I am happy to report that I have had zero VT episodes, nor any other serious arrhythmias since the ICD was installed.
But my story is not quite over. Despite the lack of arrhythmias, my running performance has not returned to pre-sarcoidosis levels. I’ve worked with the Stanford cardiology team who have reiterated that my heart is working perfectly. With that ruled out, I asked for a referral to their pulmonary team to see whether there might be some lung function issues that are interfering with my return to normalcy. Like with my heart, I undertook a battery of tests looking for anything unusual.
The results of all these tests were that my lungs, despite a lifetime of asthma are working quite well. The penultimate step in this battery was a cardiopulmonary exercise test (CPET) that is most commonly used to test professional athletes. Despite my running complaints, the tests showed that my body was responding fairly well to exercise as I posted a 12.2 MET (Metaboloic Equivalent of Task).
I studied the voluminous data from the CPET and was struck by one thing– max heart rate. No, not the calculated 220-<age> that most runners are familiar with, but rather seeing that my heart rate levels off at 149 bpm and can go no higher no matter the stress. This is Father Time making his presence known. The reason I can no longer run as fast as I used to is because my heart can’t pump fast enough to generate the required oxygen to propel my body at those speeds. It's basic physics, so simple.
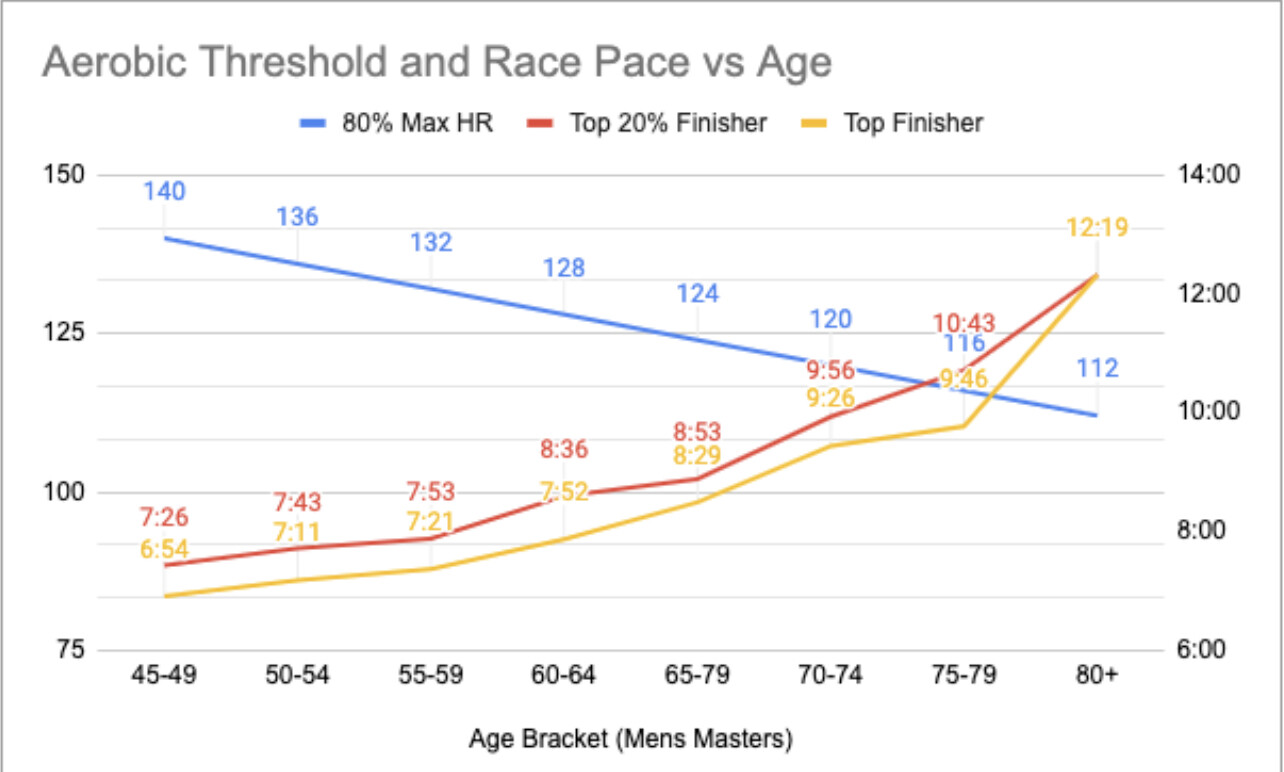
I decided to investigate this briefly and look at some representative races to see if I could see this in actual race data. I looked at the data from the California International Marathonfrom 2022 curious to see an age-related pattern. During my short racing career, I would typically place in the top 20% of my age bracket. I extracted data for Mens Masters into a chart to show Max HR vs. the top finisher and the top 20% finisher. This has given me some consolation that the slowdown is natural and will continue.
One more thing I’d like to share, especially with older runners. Since the ICD, I have found it hard to rebuild my aerobic base. I’ve concluded that the reason for this is that I was still trying to train like when I was a teenager back when my Max HR was 200! Somewhere in my memory banks, I recalled something about low heart rate training and quickly found the MAF methodby Dr. Phil Maffetone. In a nutshell, Maffetone advises training at ultra-low heart rates (180-<age>) to develop a core aerobic base. The process can take 3-6 months and involves running at an agonizingly slow pace (at first.) I am happy to report that this is the one thing that is working for me and for the first time in a long time I am again running with joy.
This has been a very personal story but one that I thought I should share with our running community. I feel that running may have saved my life. If I hadn’t challenged my doctors that I was not “fine” the worst could have happened. We runners know our bodies better than anyone and when something doesn’t feel right, it’s probably not. Don’t be afraid to aggressively advocate for yourself. Your life might depend on it.
by Warren Savage
Login to leave a comment




