Running News Daily
Running News Daily is edited by Bob Anderson. Send your news items to bob@mybestruns.com Advertising opportunities available. Train the Kenyan Way at KATA Kenya and Portugal owned and operated by Bob Anderson. Be sure to catch our movie A Long Run the movie KATA Running Camps and KATA Potato Farms - 31 now open in Kenya! https://kata.ke/
Index to Daily Posts · Sign Up For Updates · Run The World Feed
Why Altitude Training Helps Some but Not Others
A new analysis casts doubt on the idea that people are born as "responders" or "non-responders" for training in thin air
To understand the latest data on altitude training for endurance athletes, it’s worth looking back at a seemingly unrelated study published in 2015. In it, 1,000 subjects undertook a three-month exercise program to see whether it would lower their blood pressure. Sure enough, the average change in diastolic blood pressure was a clinically significant reduction of five mmHg, which is good news. But not everyone benefits equally. Here’s what the individual results looked like, with positive and negative changes in blood pressure shown on the vertical axis:
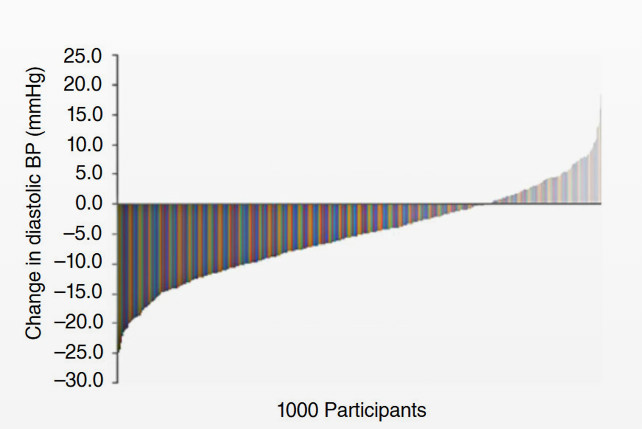
On the left, some of the subjects—call them super responders—saw a drop of more than 20 mmHg. On the right, we have some non-responders, and even some negative responders, whose blood pressure increased by more than ten mmHg. That’s bad news, and receiving it might understandably tempt you to sign up for one of those genetic tests that promises to tell you how you’ll respond to exercise.
Here’s the catch: this data is fictitious. It was generated by researchers to illustrate what can go wrong when you try to classify people as responders or non-responders based on a single set of measurements. They took simulated blood-pressure data and subtracted exactly five mmHg from everyone’s baseline value. But to simulate real-world conditions, they also added some random measurement error to both the pre and post values. For some people, their apparent baseline measurement was a little higher than its true value; for others, it was lower. Same for the final measurement. If you got a randomly low baseline and a randomly high final value, it looked like you were a non-responder—even though everyone in the simulated study was really a true responder.
This question of response and non-response has been a controversial topic in exercise science (and health more generally) for at least a few decades. Researchers have rightly realized that individual variation is just as important as the average response to an intervention. But that creates a temptation to label everyone in a study who doesn’t respond as a non-responder. It’s like flipping ten dimes and saying, “Look, dimes always land on heads, as long as you ignore those five non-responders.”
Which brings us back to altitude training. Ever since the first live-high, train-low protocols were devised back in the 1990s (with an initial study that saw 17 out of 39 subjects improve their 5,000-meter times), there’s been a widespread belief that some people are responders and others non-responders. I’ve lost count of the number of times I’ve seen secondhand altitude tents for sale on running message boards or chat groups with a note along the lines of “I tried it for a few months, but it turns out I’m not a responder.”
But, as noted above, you can’t actually sort responders from non-responders based on a single stint at altitude. To their credit, altitude researchers have been trying for several decades to identify the factors that predict whether you’re likely to see an increase in oxygen-ferrying hemoglobin, which is the main goal of altitude training for endurance athletes. But the results have been mixed at best, and it’s still not at all clear if an athlete who responds to one altitude camp will respond again to the next one.
That’s the long-standing controversy addressed by the latest altitude-training data, which is published in the Scandinavian Journal of Medicine and Science in Sports. It comes from a group led by Ari Nummela of Finland’s Research Institute for Olympic Sports, and it reanalyzes data from 59 national-team endurance athletes (cross-country skiers, runners, swimmers, and assorted others) who completed a total of 82 altitude-training camps between 2009 and 2015. The camps lasted between 16 and 42 days, at altitudes of between 4,400 and 8,200 feet (1,350 and 2,500 meters).
“Success” was defined as an increase in total hemoglobin mass of greater than 1.7 percent, which exceeds the typical error inherent in the measurement of hemoglobin mass. Overall, athletes had successful camps in 46 of the 82 cases, for a hit rate of 56 percent. That may seem unimpressive, and (as I wrote earlier this year) some scientists would argue that you’d see something similar if you simply sent the athletes to a super-focused training camp at an idyllic sea-level location, no altitude required. But if you assume that altitude works, then you’re left with two possibilities: either some athletes aren’t wired to respond to altitude, or half of them were doing something wrong.
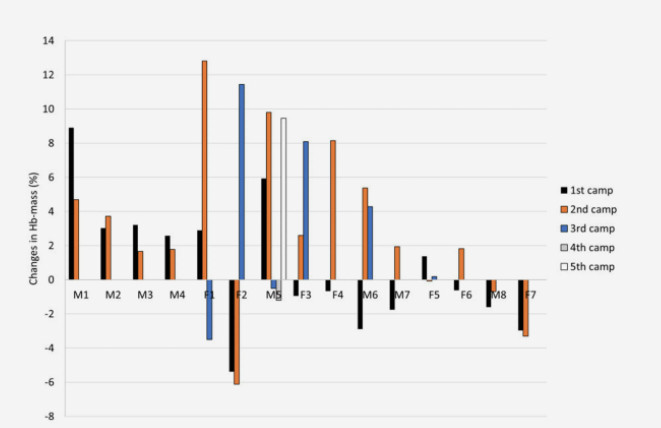
To address the first possibility, we can look at the 15 athletes who participated in at least two (and as many as five) altitude camps during the study period. Did those who benefited once consistently benefit again? Here are the individual results for those 15 athletes, with upward bars indicating an increase in total hemoglobin and downward bars indicating a decrease:
Four of the athletes (on the left) always benefited, and two of them (on the right) always saw neutral or negative responses. For the other nine, it was a mixed bag. Subject F1 had two good camps, then a bad one; subject F2 had two terrible ones, then an amazing one. The firm conclusion here, Nummela and his colleagues write, is that altitude response is not a fixed trait.
The harder question, then, is: What determines whether you’re going to have a successful camp? One solid finding was that the success rate jumped to 65 percent when the altitude was at least 6,500 feet (2,000 meters). As it turns out, the authors of this paper were the ones advising the Finnish national team on its altitude camps, and they can’t resist pointing out that this is exactly what they originally told the national-team coaches to expect. But did the coaches listen when they chose their altitude-training destinations? Apparently, not always.
The physiologists also had two other pieces of advice for the coaches: don’t let your athletes come to altitude if they have low iron stores (defined as serum ferritin below 30 micrograms per liter) or if they’re ill (as indicated by levels of the inflammation marker C-reactive protein above three milligrams per liter). These rules, too, were not enforced, so the researchers checked whether those with low iron or high inflammation were less likely to respond. The results were unconvincing: if anything, the non-responders had slightly higher baseline ferritin and lower C-reactive protein than the responders.
Other studies, in contrast, have found that having good iron levels and avoiding illness are crucial to getting good results from an altitude camp. And the physiologists who work closely with elite athletes have plenty of other ideas about what it takes to ensure a successful training block in thin air. The real conclusion, yet again, is that getting the most bang out of your altitude buck is complicated and highly individual. You can take that as a glass half empty: simply booking a plane ticket guarantees nothing. Or you can take it as a glass half full: even if your first stint at altitude didn’t work out, you might still be able to make it work the next time—if you get the details right.
by Outside Online
Login to leave a comment




