Running News Daily
Running News Daily is edited by Bob Anderson. Send your news items to bob@mybestruns.com Advertising opportunities available. Train the Kenyan Way at KATA Kenya and Portugal owned and operated by Bob Anderson. Be sure to catch our movie A Long Run the movie KATA Running Camps and KATA Potato Farms - 31 now open in Kenya! https://kata.ke/
Index to Daily Posts · Sign Up For Updates · Run The World Feed
Exercise and the Immune System
There seem to be two groups of people, those who “never get sick” and those who are chronically under the weather. Over the years, I have been a member of both camps. While I have previously suffered from overtraining syndrome and had what felt like chronic upper respiratory infections–which I wrote about in this RunFar article–I have more recently (and despite teaching high-school kids) avoided colds, flus, and other bugs. I’m sure writing that sentence will cause me to soon fall ill, though!
Why do we seem to get sick more often sometimes, and less sick in others? How does our immune system work to protect us from illness? And in what ways does exercise impact our immune system’s function? These are important questions for a community that enjoys pushing our bodies, sometimes in fairly extreme ways.
The Basics of the Immune System
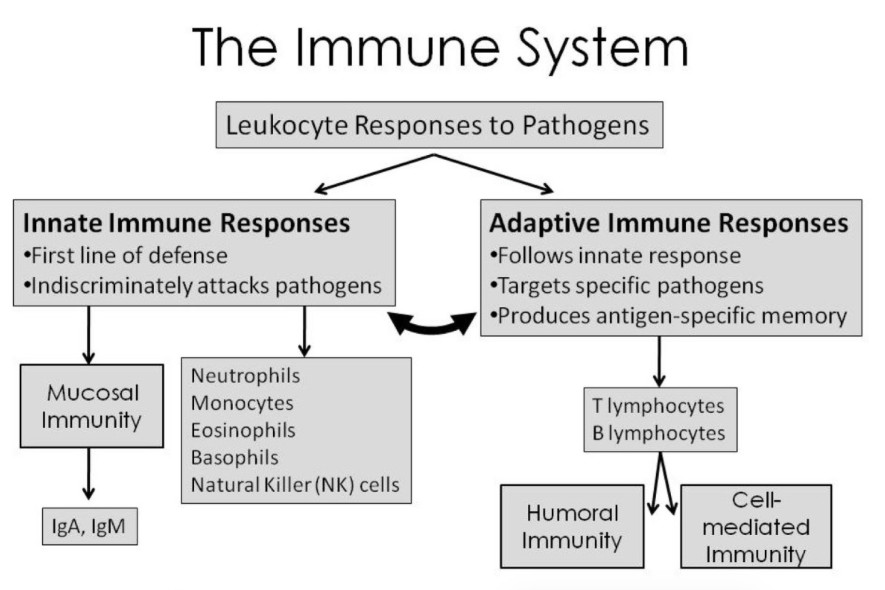
I’ve mentioned this before and I think it’s worth mentioning again now: the human body is an incredibly clever system that works surprisingly well most of the time! One particularly clever element is our immune system. The immune system’s job is to protect you from outside intruders such as antigens (any toxin or foreign substance), including pathogens (bacterium, virus, or microorganism that can cause disease). Your immune system is broken into two main responses: innate immunity which is often referred to as non-specific immunity and adaptive immunity which is known as specific immunity
graphic showing how the immune system is broken down into two major response types, innate and adaptive immunity, and what those responses involve. Image: Hackney, A. C. (2013). Clinical management of immuno-suppression in athletes associated with exercise training: Sports medicine considerations. Acta Medica Iranica, 51(11), 751–756.
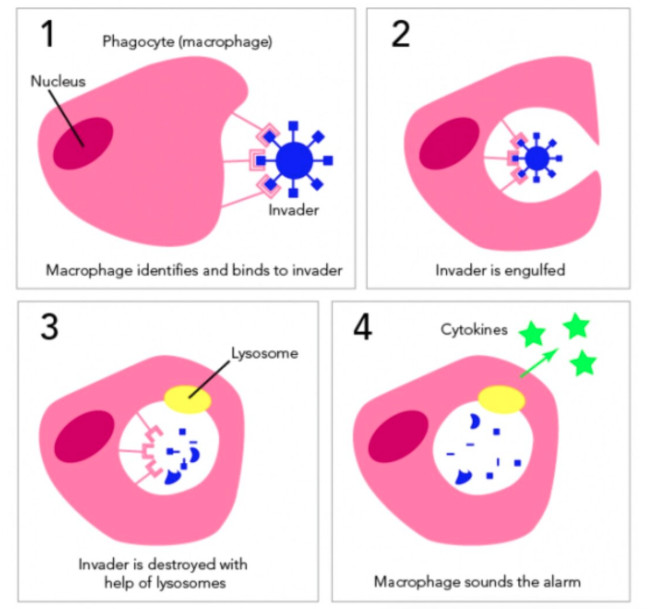
The innate immune system is referred to as non-specific because it mounts the same response each time no matter the type of intruder. The innate immune response includes what are known as your first and second lines of defense. The first line of defense includes not only physical barriers like your skin, but also chemical defenses like sweat, stomach acid, tears, mucus linings, and saliva. The second line of defense can be considered a chemical defense, in this case involving a variety of white blood cells. The white blood cells primarily responsible in the innate system are called neutrophils and macrophages. Both of these cell types are phagocytes, which means their job is to protect us via the process of phagocytosis (engulfing and digesting things that do not belong).ow a macrophage (the biggest of the phagocytes) identifies an intruder, engulfs it, and then uses enzymes in its lysosome to “digest” the invader. The macrophage then releases “signals” (in the form of cytokines) to sound the alarm to other cells. Image: Letstalkscience.ca/educational-resources/stem-in-context/immune-response
The adaptive immune response, called the specific response and the third line of defense, is a more complex chemical response because of how it learns to identify different antigens and is acquired over our lifetime starting from the moment we make our entrance into this world. Like the innate immune response, the adaptive response utilizes white blood cells to identify and destroy intruders, this time relying on a type of white blood cell called a lymphocyte. Lymphocytes are special in the sense that they develop memory when exposed to antigens, so that when you are exposed to them again your body is better prepared to fight them off. We develop our adaptive immunity from both natural exposures to antigens over the course of our lifetime and via other exposures like vaccines.
Moderate Aerobic Exercise is Good for the Immune System
Despite the field of exercise immunology being a relatively new area of scientific study with 90% of papers published after 1990, original studies date back over a century (4). Early research focused specifically on exercise-induced changes in cell counts (how many white blood cells were present before and after exercise of different intensities). From this vast body of scientific literature, we know that daily moderate exercise (up to 60 minutes of easy aerobic exercise) provides an overall “boost” to our immune system’s function, increasing our resistance to mild infections like the common cold (8). This is due to the enhanced recirculation of immunoglobulins (proteins that help recognize specific antigens), anti-inflammatory cytokines (molecules that help regulate inflammatory response), neutrophils (part of our innate immune response), and lymphocytes (part of our adaptive immune response) (4).
Can Exercise Be Bad for the Immune System?
If 60 minutes of aerobic exercise is good for our immune system, then is more better? It’s quite possible that you’ve become sick shortly after a big effort or goal race, and that’s exactly what researchers have found in widely published studies in the 1980s continuing through the present. These studies illustrate that infectious episodes (reported upper respiratory infection [URI] symptoms) increased after taking part in large endurance events. This includes a study from the 1982 Two Oceans Marathon–actually a 56-kilometer ultramarathon–where one third of the participants self-reported URI symptoms within two weeks of the race (4, 5). This and many other studies (generally conducted on major road marathon participants) helped to form the idea behind an exercise immunology theory known as the open window theory (5, 6).
The open window theory is the idea that after an intensive exercise session (either a long or hard effort) there is a period of time, generally three to 72 hours, where you have an increased susceptibility to illness. This was supported by what appeared to be a dramatic falloff of circulating lymphocytes (in particular natural killer cells, a subset of lymphocytes called T cells) post-exercise (1, 2). These values were shown to be as much as 40% below baseline cell counts (2). This was concerning because the initial studies reporting this rapid lymphocyte reduction also reported large rates of cell death (2).
That sounds bad. Well, those initial cell-death values were never substantiated–phew!–but where are the lymphocytes going if they are not dying? It turns out that lymphocytes are believed to shift to more peripheral locations in the body where they are more likely to encounter an antigen, such as in the lungs or gut (2). Think of this as white blood cell redeployment in which there is enhanced immune surveillance following strenuous exercise.
What Should Athletes Do to Decrease Illness Risk?
If we know that multiple factors influence our immune systems, what can each of us do to make sure our immune system functions properly? Address those factors!
Monitor your exercise workload. Adequate stress plus adequate rest equals optimal physiological improvement. But when this is thrown out of alignment and physical stress accumulates without appropriate rest, impairments in your immune system function may occur and result in an increased risk of getting sick (8). Regular exercise is good for your immune system, but a training load that is too high for too long can take its toll. Be sure to read our article on overtraining syndrome to learn more about the stress-rest balance.
Consider fueling strategies during exercise and avoid overall nutritional deficiency and caloric restriction. The scientific literature suggests that ingesting carbohydrates during prolonged or intense activity is associated with reduced stress hormones and reductions in inflammation. Additionally, maintaining a balanced and diverse diet that meets your needs and energy demands to match your training, including proper hydration, is important (2).
Practice good hygiene. Avoid close contact with individuals who are or have been sick recently, frequently wash your hands throughout the day, and avoid touching your face (nose, mouth, and eyes).
Practice stress management. Although short-term stress (like exercise) might have a positive effect on your immune system, chronic stress does not. Chronic stress can suppress your immune responses by decreasing the numbers and functionality of lymphocytes, and dysregulating your innate and adaptive immune responses (7).
Get adequate sleep. Sleep disturbances can depress your immune system, increase inflammation, and promote other poor health outcomes. Aim for seven to nine hours of sleep a night. Learn more about how sleep and your immune system interact in our in-depth sleep article.
Evaluate your touchpoints with others. Be considerate of how you interact with the world around you, including at running events and races. Consider fist bumps over high fives, be considerate of how you interact with race volunteers, and minimize what you touch at aid stations. (I have a habit of touching everything.) Be cognizant of not only your own health, but also the health of others. Practicing good hygiene isn’t limited to only when it’s convenient.
by I Run Far
Login to leave a comment




