Running News Daily
Running News Daily is edited by Bob Anderson. Send your news items to bob@mybestruns.com Advertising opportunities available. Train the Kenyan Way at KATA Kenya and Portugal owned and operated by Bob Anderson. Be sure to catch our movie A Long Run the movie KATA Running Camps and KATA Potato Farms - 31 now open in Kenya! https://kata.ke/
Index to Daily Posts · Sign Up For Updates · Run The World Feed
Can Exercise Replace Your Antidepressant?
Some doctors are now prescribing physical activity for mental health. Here's why.
For centuries, we’ve known anecdotally that movement can improve your mood. Joggers often describe a euphoric runner’s high, while swimmers recall an inner calm that lasts long after they leave the pool. In April, researchers published the strongest evidence to date showing that physical activity does more than induce these temporary feel-good effects; It can actually improve depression as effectively as medication or psychotherapy. The findings build on previous studies showing exercise can reduce anxiety, post-traumatic stress disorder, bipolar, and obsessive-compulsive disorder symptoms.
This mounting evidence doesn’t suggest you should toss out your medication or skip your next therapy appointment in favor of exercise alone. But it does indicate physical activity could be a powerful first-line treatment for mental health disorders, especially when combined with other therapies.
Based on the data, some experts see exercise as a safe, cheap antidepressant that could help the estimated one third of adults with mental illness who do not receive adequate treatment. And some clinicians are putting this concept into practice, doling out “exercise prescriptions” for mental health. These scripts give patients step-by-step instructions for physical activity recommendations, much like they would with antidepressants or behavioral therapy. But providers say that on the whole, the field has been slow to embrace exercise as medicine for mental illness, and “exercise prescriptions” remain the exception in clinical care, not the norm.

“Exercise is a good, underutilized tool to help with mental health conditions,” Ivan Escobar Roldan, a psychiatrist in Florida who regularly writes “exercise prescriptions” for his patients and studies the use of exercise in clinical practice, says. He co-authored a study published in the Journal of Psychiatric Practice in 2021 showing that while many providers generally encourage patients to be active, they don’t often give specific instructions due to a lack of training, education, or standardized clinical guidelines.
“Everyone says you should exercise more,” Seattle-based clinical psychologist Julie Vieselmeyer says. “But patients always ask: What does that mean? Do I need to take an extra lap around the grocery store, or does that mean I have to go to a gym for three hours every day?”
Currently, mental health providers don’t give the clearest answers to these questions.
Exercise is as close to a miracle drug as we’ve got. Research shows it works as effectively as some prescription drugs in preventing and treating more than 26 different diseases.
When you start a workout, your pulse quickens and breathing deepens as your heart pumps oxygen-rich blood to your brain and muscles. Within a few minutes, you likely notice a lift in your mood as your brain releases “happy chemicals” like endorphins, dopamine, and serotonin (the same neurotransmitter targeted by antidepressants). The fleeting bliss of a runner’s high results from a spike of endocannabinoids in the bloodstream—cannabis-like signaling molecules that are naturally produced in your body and induce feelings of calm.
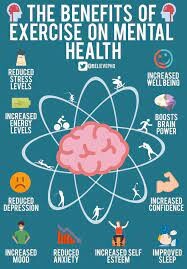
After your strength or conditioning session wraps up, the positive effects don’t stop. Over time, physical activity can increase levels of a protein called brain derived neurotrophic factor (BDNF), which leads to the creation of new neurons. More BDNF is correlated with reduced anxiety and depression, better focus, improved cognition, and sharper memory as you age.
When people exercise regularly, the brain’s hippocampus—the area linked to memory and learning—has also been found to increase in volume. That’s not all. With a regular workout routine, people often feel better, sleep better, eat better, and report improved relationships and work satisfaction. Exercising can burn off anxious energy as well as increase resilience to future stress. Eventually, it can even help people taper off medication and cut down on doctor’s visits or medical treatments. People who start to exercise before or during middle age typically save between $824 to $1,874 annually on their health care costs after retirement.
“While medications may take a few weeks to work, you see benefits right away with exercise,” Escobar Roldan says. “It’s not only going to help with anxiety, depression, and many other mental health conditions, but also with patients’ overall health and other chronic conditions.”
Getting moving can be tough initially. Despite the upsides, less than a quarter of U.S. adults do enough aerobic exercise or strength training to meet the national physical activity guidelines. But once people get going, exercise’s instant gratification often kicks off a beneficial feedback loop, Vieselmeyer says.
“When we’re making healthy choices, that ends up affecting how we think about ourselves, our self-confidence, and our energy levels—things affect our emotions positively and lead to behavior change,” she says. Working out isn’t just about quelling anxiety, depression, or negative emotions, but fostering positive ones too.
Matthew Ellison, a late-twenties investment banker based in New York City, has experienced these benefits firsthand. Ellison has a history of anxiety and recently dealt with a bout of depression tied to work stress. With the support of his therapist, Ellison made going to the gym a daily priority. He says the routine pulled him through this period and has become a non-negotiable practice to maintain his mental health.
“Being able to clear my mind, in the morning or late at night, has honestly been the greatest thing for my mental health,” Ellison says. “It’s the foundation for my mental well-being.”
For more than 20 years, Vieselmeyer has been interested in exercise as medicine, and says that amid recent studies, she is seeing more acceptance of the topic across the field. But even with a robust body of evidence, providers still struggle to convert these research breakthroughs into targeted exercise prescriptions.
That’s because there’s little formal training or education on the topic. Some clinicians are concerned about their patients’ health status and worry that exercise might lead to injury or cause a heart attack. Others simply don’t have the time to discuss exercise in depth.
Many providers recommend 150 minutes (or 2.5 hours) of physical activity per week—guidelines from the U.S. Department of Health and Human Services—but are hesitant to give concrete instructions beyond that. The American Psychological Association’s most recent clinical practice guidelines on depression don’t mention exercise as treatment.
In his own practice, Escobar Roldan uses resources like this prescription form created by Exercise is Medicine, a global initiative coordinated by the American College of Sports Medicine. The organization also provides a handy action guide to help providers prescribe the right “dose” of physical activity for more than 40 chronic conditions, including mental health disorders. Exercise is Medicine maintains a referral program for health professionals to connect patients with qualified exercise professionals. Some insurance companies also subsidize training programs or gym memberships, or even reimburse health and fitness expenses. But these programs aren’t yet commonly used in the mental health arena. “You need a lot of mounting evidence to see a paradigm shift or clinical practice change,” says Escobar Roldan. “With more awareness, we’re moving towards that, but we aren’t there yet.”
To get patients moving, Vieselmeyer and Sarah England, a clinical psychologist based in New York, don’t use strict “prescriptions.” Instead, they draw on techniques from cognitive behavioral therapy, one of the most evidence-based forms of therapy. The psychologists use motivational interviewing to explore the root causes of behavior and barriers to exercise. They also target behavioral activation, which uses behavioral shifts like physical activity to influence people’s emotional state.
“If clients are severely depressed and unable to do their laundry, I’m not going to suggest running two miles,” England, who helps patients set “SMART” goals that are specific, measurable, achievable, relevant, and time-bound, says. “We have to behaviorally activate them first, in smaller steps, like walking around the block.”
Ellison managed to establish a regular workout routine with only vague encouragement from his therapist. But for many others dealing with mental health issues, symptoms like fatigue or lack of motivation preclude their ability to exercise regularly.
“When somebody is really depressed, it’s hard to put the running shoes on and get out the door, even if they know that’s going to make them feel a whole lot better,” Vieselmeyer says. Sometimes the easiest entry point might be medication or seeing a therapist, and then progressing to exercise, she says.
Much of the evidence behind the antidepressant and anti-anxiety effects of exercise is based on people with mild to moderate cases of mental illness. A few small studies suggest that structured workout treatments can help patients with serious mental illness in inpatient settings. But on its own, exercise is unlikely to alleviate serious mental illness, experts say.
A major reason why mental health providers have been slow to embrace exercise as treatment is because researchers haven’t nailed down the exact “dose and effect” like they would with a prescription drug. More research is needed to determine which type of exercise works best, how much is needed, and who it can benefit mentally.
Based on what we know so far, the most effective exercise prescription includes physical activity that is:
Escobar Roldan suggests people bring their heart rate up to the point where they are a little bit out of breath. Gardening, walking, dancing, hiking, running, or cycling can all ease symptoms of anxiety and depression.
Most studies point to aerobic exercise as a way to boost your mood, but evidence shows strength or resistance training works too. It’s more about getting people moving doing something they enjoy, rather than finding the “perfect” exercise, Vieselmeyer says.
Group exercise sessions, from bootcamp to yoga, can be especially effective. People appear to gain more benefit when supervised by trained health and exercise professionals. There’s also the extra opportunity to connect with others, which pays dividends on our mental health.
Vieselmeyer recommends starting small. No triathlon or two-a-days involved. It’s more about working out consistently, not calculating the perfect ratio of Crossfit to Pilates.
“Whatever prescriptions are made going forward need to fit with people’s lives, or they’re just not going to do them,” Vieselmeyer says. “There are already enough barriers for people to exercise.”
Ultimately, physical activity isn’t a silver bullet for mental health—and more intense movement isn’t always the best strategy, especially for fitness fanatics who already train hard. “A good long run is not enough to process through your history of trauma,” Vieselmeyer says. If exercise alone was the panacea to our mental health crisis, we wouldn’t see any mental health difficulties in professional athletes, England notes.
The right exercise prescription comes down to each person’s level of physical and mental fitness. “I certainly hope no one is hesitating to prescribe exercise on top of other evidence-based treatments,” Vieselmeyer says. “I would rather give patients more tools than fewer, and then see where their interest lies.”
by Outside Online
Login to leave a comment




